08:00
What does segregation do in infection processes?
EPID 684
Spatial Epidemiology
University of Michigan School of Public Health
Jon Zelner
[email protected]
epibayes.io

Today’s Theme
Making mechanistic sense of linkages between structural inequity and infection.
Agenda
The persistent myth of the equal opportunity infector and its impact on epidemiological models.
How can we better measure the mechanistic impact of structural racism on inequity in disease outcomes?
Does (1) provide any clues about how to build better models?
What are the challenges and risks of trying to account for structural racism in disease outcomes?
In pairs:
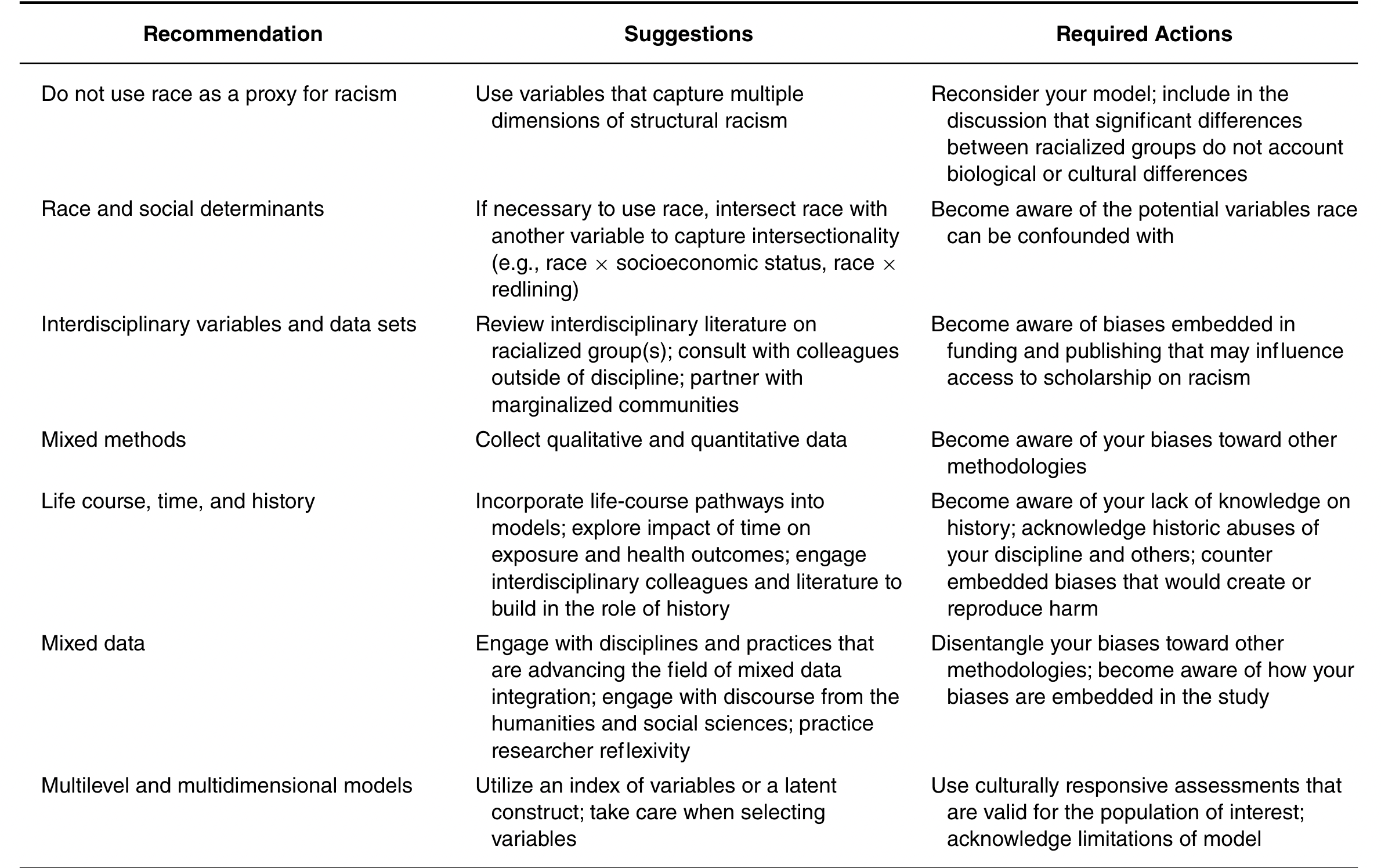
What pitfalls do (2) identify to characterizing structural racism in epidemiological analyses?
Of their suggestions, which seem most actionable or compelling to you?
What challenges do you see in effectively implementing this vision?
Modeling infection inequity
Modeling has become a key element of pandemic preparedness.
“Pandemic preparedness is a continuous process of planning, exercising, revising and translating into action national and sub-national pandemic preparedness and response plans. A pandemic plan is thus a living document which is reviewed regularly and revised if necessary…based on the lessons learnt from outbreaks or a pandemic, or from a simulation exercise.”
Much of the power of models comes from how they shape our intuition
Models can let us:
- Characterize rates of transmission, severe disease and death in different populations and locations.
- Estimate impacts of medical interventions on risk over space and time.
- Explore the implications of social and political change on the spatial and social distribution of infection risk.
Intuition pumps are cunningly designed [thought experiments, which] focus the reader’s attention on “the important” features, and…deflect the reader from bogging down in hard-to-follow details. (From Dennett, 1984)
Early pandemic models focused on key priorities
- Spatial variation in risks of infection and death.
- Age-specific incidence and mortality.
- Community-level hospital and ICU capacity.
- Short-term forecasting of population incidence and mortality
- Localized impacts of lockdowns on infection risk.
- Economic and racial inequality in infection and disease risk
Economic and racial inequity is a central story of the COVID-19 pandemic





So why were we not prepared for these easy-to-foresee inequities?
The myth of the equal opportunity infector may have obscured inequality

What does it mean to be an equal opportunity infector?
Susceptibility is uniformly distributed across the population.
Host and pathogen biology are the most important factors in determining infectiousness.
Protective health behaviors equally available to everyone.
Socio-spatial differences in exposure by race and wealth are dwarfed by these biological factors.
Modelers don’t have to believe these things are true for them to end up in our models!
We have to understand the mental models guiding our mathematical ones to figure out how to fix them.
[M]ental models and empirical data keep each other in check - [Sir Peter Medawar] described them respectively as the ‘bride’ and ‘groom’ of science — and scientific progress in any discipline occurs by the back-and-forth dialogue between their two ‘voices’.”
From Greenhalgh 2021: Miasmas, mental models and preventive public health
Dissecting the mental model behind the equal opportunity infector idea
Key Questions:
- What types of data do these models use? Why?
- Who has been the typical audience for epidemiological models? Is that changing?
- What can we do to expand our toolkit to address these critical questions?
Who are epidemiological models for?
- Public health officials making decisions.
- Scientists and physicians pursuing interventions.
- Politicians implementing policy and trying to maintain power.
- Media constructing an easily-digestible narrative.
What perspective do these groups have in common?
This has led to a focus on a set of outcomes that aligns with these interests
- Incidence of disease over time.
- Prevalence of infection at any given moment in time.
- Mortality and case-fatality rates.
- Distributions of infection and mortality by age.
- Distribution of infection and mortality by neighborhood, socieconomic status, and race/ethnicity.
Modeling of acute infections has emerged from a rich tradition in population ecology
Key model parameters like \(R_0\) traditionally describe average properties of infection in a well-mixed population.
Key ideas are borrowed from classic models of predator/prey dynamics and birth/death processes.
Ecological modeling has an extensive toolkit for characterizing demographic and spatial variation in outcomes.
But we have been slow to make the leap to characterizing the socio-structural determinants of infection.
OK, but this was so obvious!
Historical analyses have repeatedly demonstrated inequity in prior pandemics
The mechanisms of inequity were quickly identified, but our models weren’t ready for them
The good news is that these models are not carved in 🪦 stone 🪦
COVID-19 disparities are not the fault of those who are experiencing them, but rather reflect social policies and systems that create health disparities in good times and inflate them in a crisis. The US must develop a new kind of “herd immunity,” whereby resistance to the spread of poor health in the population occurs when a sufficiently high proportion of individuals, across all racial, ethnic, and social class groups, are protected from and thus “immune” to negative social determinants.
From Williams & Cooper, “COVID-19 and Health Equity—A New Kind of “Herd Immunity”, JAMA, 6/23/2020
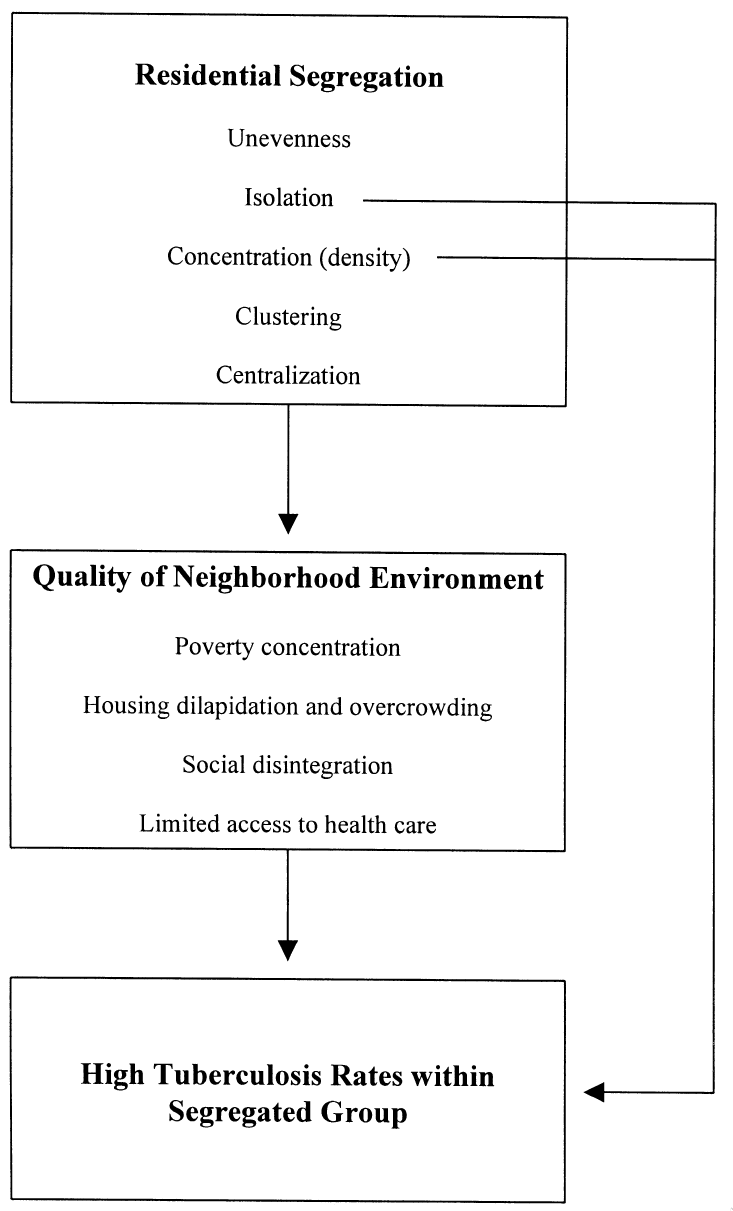
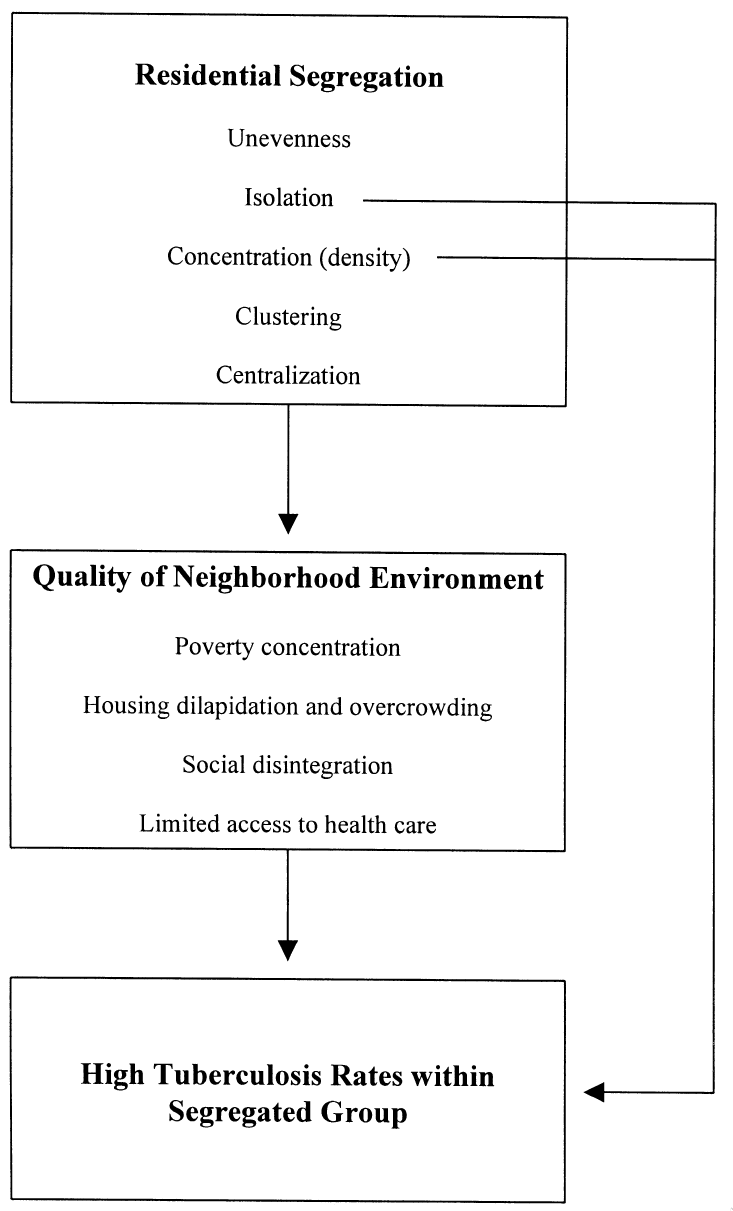
What might an alternative framework look like?
- Model spatially localized infection risks as a function of upstream social determinants.
- Represent correlation between effects of factors such as racism and SES on spatial variation in infection risks.
- Examine differential impacts of social inequity on contact, susceptibility, and infectiousness.
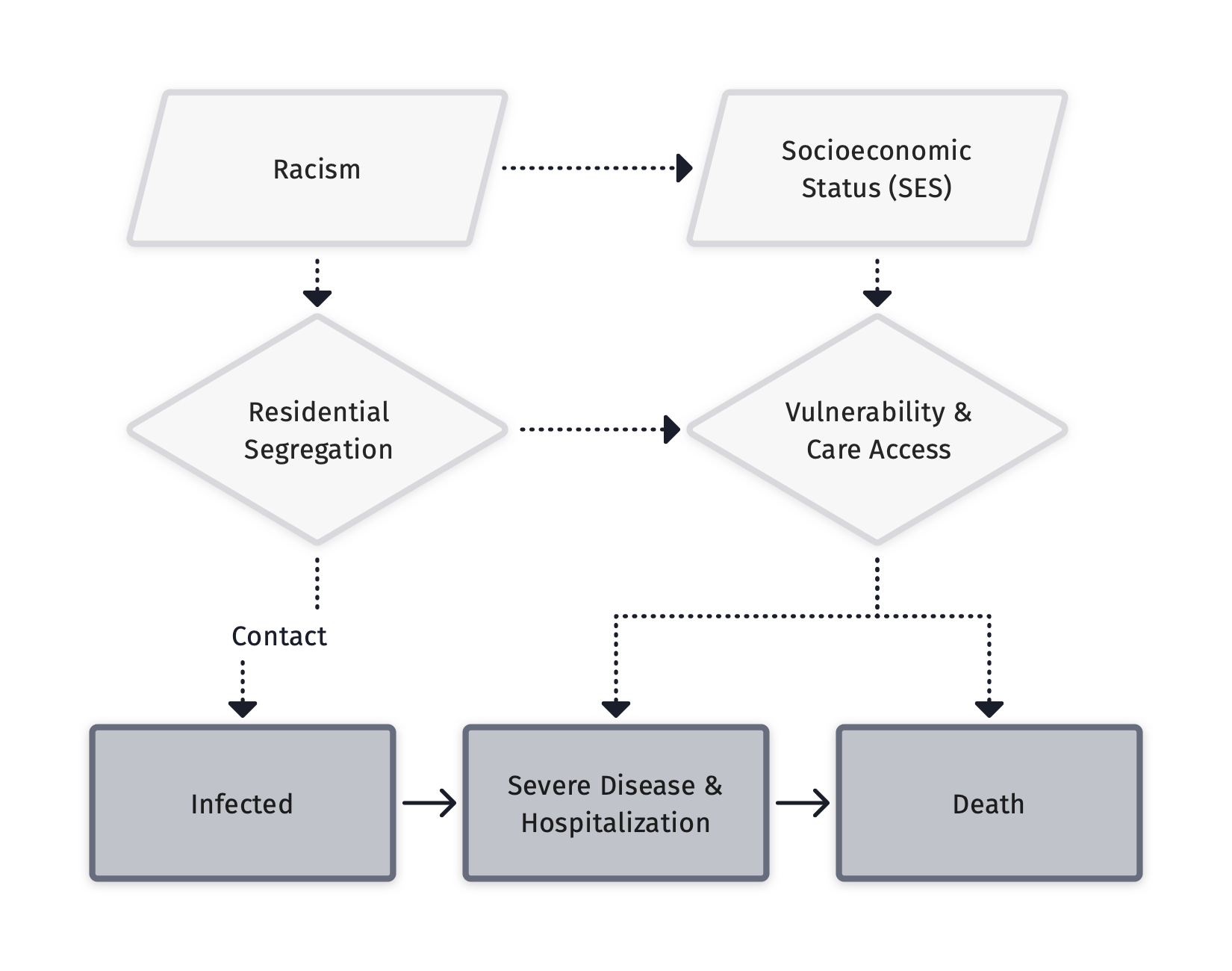
Zelner et al. (2022), There are no equal opportunity infectors. PLOS Computational Biology
This shift is already well underway
And it reflects recent experiences as well as ideas that have been bumping around for awhile
These equity-oriented models let us ask crucial questions about the causes of disparity
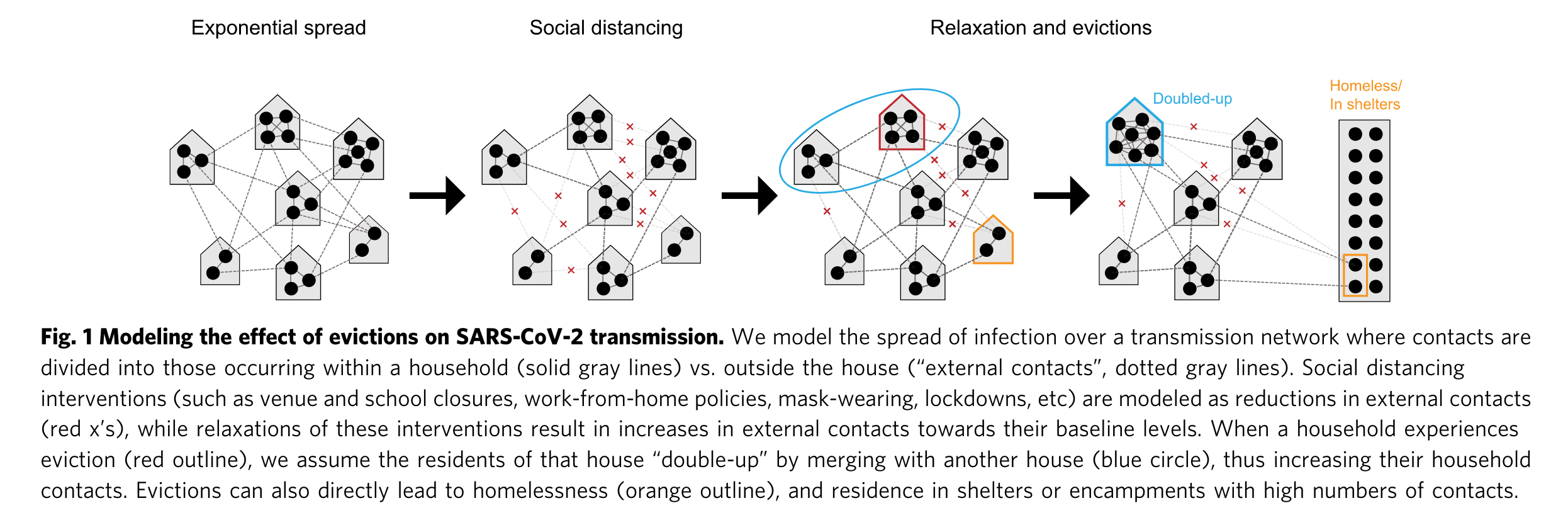
From Nande et al. “The effect of eviction moratoria on the transmission of SARS-CoV-2”, Nature Communications, 2021
OK: Here’s my stab at doing a better job of modeling the drivers of inequity in infection risks
Hands-on with a mechanistic version of this model
Next Time
Workshop!